Each month, The Clinical Advisor makes one new clinical feature available ahead of print. Don’t forget to take the poll. The results will be published in the next month’s issue.
Each month, The Clinical Advisor makes one new clinical feature available ahead of print. Don’t forget to take the poll. The results will be published in the next month’s issue.
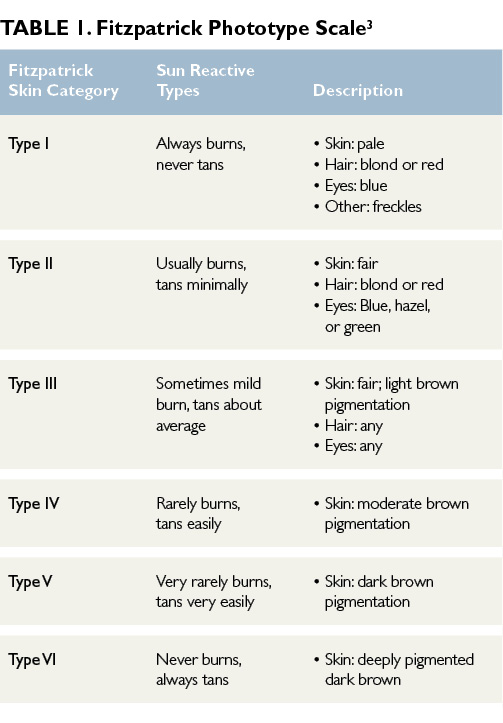
Actinic keratoses (AKs) are one of the most frequently encountered skin lesions in clinical practice.1,2 AKs are precancerous, focal, sun-induced areas of abnormal proliferation of atypical keratinocytes confined to the lower layer of the epidermis.1,2 Often referred to as solar keratoses, these lesions commonly occur in areas with chronic and cumulative sun exposure such as the face, ears, neck, dorsal forearms, hands, and scalp.1,2 The highest incidence of AK is seen in middle-aged to elderly men with chronic and sustained ultraviolet (UV) radiation exposure over their lifetimes. AKs are more prevalent in fair-skinned individuals and those categorized as Fitzpatrick skin types I and II (Table 1)3; the Fitzpatrick phototype scale is a numerical classification used to estimate the response of different types of skin to UV light.3
Etiology/ Histology
The main mechanism of AK formation is prolonged sun exposure and cumulative exposure to UV radiation.4 AKs result from the adverse effects of UV-A and UV-B light radiation on keratinocyte DNA.2,5 UV radiation induces cellular mutations and results in the formation of atypical keratinocytes.2,5 Mutations of genes may cause impaired apoptosis, uncontrolled cell proliferation, and progression to invasive squamous cell carcinoma (SCC).1,6 Although most AKs remain superficial and confined to the epidermis, some lesions will penetrate the reticular or papillary dermis and differentiate into SCC, especially when multiple AKs are present.1,6
Which of the following is the least effective topical therapy for actinic keratoses?
Clinical Presentation
The classic presentation of AKs is a gritty macule or small papule, varying in size, with an erythematous base and an overlying scaly white patch that is rough to palpation.2 Although AKs are commonly asymptomatic, patients may report occasional burning or lesion tenderness. Immunocompromised patients, specifically organ transplant recipients receiving treatment with immunosuppressive medications, are at increased risk of developing AKs.1,6 AKs may spontaneously regress, completely resolve, persist, or progress to SCC, particularly in the presence of multiple AKs.2 Clinically it is difficult to predict the course of AKs, and no method exists for predicting lesions that will evolve into invasive SCC.5 The risk of AKs transforming to SCC is minimal (1%)1; however, current guidelines suggest treating all AKs.4
Diagnosis
Diagnosis generally is made by visual inspection and palpation. Keratoacanthoma, SCC, basal cell carcinoma, and seborrheic keratosis lesions may have a similar presentation to AKs and must be considered in the differential diagnosis.2 Characteristic history and examination findings are usually adequate for diagnosing AK, but dermoscopy, if available, is recommended if the clinical exam findings are not typical of AK. A strawberry pattern, consistent with undulated vessels surrounding hair follicles filled with yellow keratotic plugs on an erythematous background, is characteristic of AK lesions on dermoscopy. Skin biopsy is performed if the clinical exam and dermoscopy findings are not typical of AK. Any clinically suspicious lesion — including lesions with increasing tenderness, rapid enlargement, or those recalcitrant to initial therapies — warrants skin biopsy for a definitive diagnosis.2
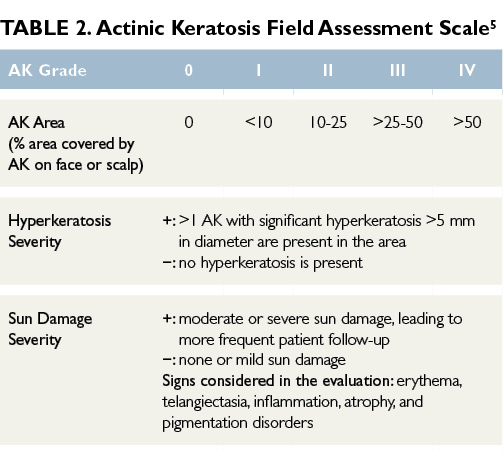
Surrounding the visible and palpable AKs lesions are skin areas prone to sun damage that are more likely to develop into clinical AKs or other sun-related cancers.5 Subclinical, nonvisible sun damage is known as field cancerization.5 Determining the severity of AKs and the extent of surrounding field damage can be challenging. Many AK grading tools use visible isolated lesion counts to assess the severity of the AKs, but they lack grading of the surrounding sun-damaged skin. The Actinic Keratosis Field Assessment Scale (AK-FAS) has been developed and tested as a relevant and reproducible assessment of AKs in clinical practice and aids in the grading of the severity of AKs and the field area damaged by UV radiation.5 Utilizing the scale can standardize a diagnosis, aid in selecting the most appropriate treatment, and provide an objective method to assess treatment response (Table 2).5